Unmasking the Hidden Causes of Why Pain Returns
Experiencing an injury is frustrating enough, but when the pain returns despite apparent healing, the feeling can quickly turn to despair. You’ve rested, perhaps undergone treatment, and started to feel better, only for the familiar discomfort to resurface, sometimes even more intensely. This cycle of relief and relapse is a common, yet often poorly understood, challenge. While initial healing may address the immediate damage, numerous underlying factors can prevent true recovery, leaving you vulnerable to recurring pain and limiting your potential. This article delves into the hidden causes behind why pain returns, moving beyond the surface to uncover the deeper issues that hinder lasting healing and performance.
The Frustration of Relapsing Pain
The journey from injury to recovery can be taxing. Whether it’s a sports-related incident, such as the 12% of sports injury hospitalizations in Australia attributed to cycling, or a workplace mishap, such as the 2.6 million nonfatal workplace injuries and illnesses reported in private industry in the U.S. in 2023, the initial phase is often focused on immediate pain management and rest. However, the reality is that in many cases, a significant portion of the population continues to struggle with pain long after the acute phase. In fact, 24.3% of adults experienced chronic pain in 2023, highlighting the widespread nature of this challenge. This persistent discomfort often stems from issues that were not fully addressed during the initial recovery period.
The Lingering Echo: When an "Old Injury" Refuses to Fade
An "old injury" that repeatedly flares up is a stark reminder that the body's healing process is more complex than it appears. Superficial healing, where acute pain subsides and basic function returns, doesn't always equate to complete tissue restoration. Subtler damage may persist, or the body may adapt in ways that create new problems. The residual effects of the initial trauma can create vulnerabilities that are easily re-aggravated by everyday activities or even minor stresses, leading to a seemingly endless cycle of pain returning.
Beyond the Obvious: Why Surface-Level Healing Isn't Enough
The frustration arises because we often assume that once the initial pain is gone, the injury is resolved. However, the body is a dynamic, interconnected system. When one part is compromised, the entire structure must adapt. This adaptation, while necessary for immediate function, can lead to long-term biomechanical imbalances and increased strain on other tissues. True healing requires restoring not just pain-free movement, but also the underlying strength, flexibility, and functional capacity of all involved tissues.
A Journey to Deeper Understanding: Unmasking the True Culprits of Why Pain Returns
To break free from the cycle of recurring pain, we must look beyond the immediate symptoms and investigate the hidden causes that keep an injury alive. These underlying factors are often less visible but profoundly impact long-term recovery and performance.
The Body's Echoes: Incomplete Healing and Persistent Damage
The initial trauma may leave behind more than just a memory of pain. Incomplete healing means that damaged tissues might not have fully regenerated or regained their original strength and integrity.
The Scars We Don't See: Problematic Scar Tissue and Adhesions
During healing, the body forms scar tissue to repair damaged muscles, ligaments, and other soft tissues. While essential for structural integrity, this scar tissue is often less flexible and elastic than the original tissue. This inelasticity can restrict mobility, create adhesions (where tissues stick together unnaturally), and force surrounding muscles to work harder. This uneven loading can lead to recurrent strains or joint irritation, essentially re-injuring the area or causing new problems.
Nerve Sensitivity and the Pain Loop
When tissues are injured, nerves in the affected area can also be damaged or become sensitized. This nerve damage can lead to altered signal transmission, where nerves begin sending abnormal pain signals, even in the absence of ongoing tissue damage. This phenomenon can create a persistent pain loop, making the nervous system hypersensitive to stimuli that wouldn't usually cause discomfort.
The Persistent Fire: Chronic Inflammation
Inflammation is a natural response to injury, but it can become chronic if not adequately managed. Factors like diet, stress, and inactivity can contribute to ongoing, low-grade inflammation that keeps tissues irritated and pain signals active. This persistent inflammation hinders proper tissue regeneration and can keep an old injury feeling "fresh" and prone to aggravation.
The Structural Story: Biomechanical Imbalances and Movement Patterns
How we move significantly influences our susceptibility to injury and re-injury. Altered biomechanics can place undue stress on specific areas, even if the original injury site appears healed.
The Tug-of-War Within: Muscle Imbalances and Compensation Patterns
When an injury occurs, other muscles often compensate to maintain function. Over time, this can lead to imbalances where some muscles become overused and tight, while others become weak and inhibited. These imbalances disrupt the body's natural alignment and can place abnormal stress on joints and ligaments, increasing the risk of re-injury or new pain sources.
The Foundation of Movement: Postural and Joint Misalignments
The spine, pelvis, and individual joints form the foundation of our movement. Even subtle misalignments in these structures can create cumulative stress over time. Such imbalances can alter gait, restrict motion, and overload specific tissues, making them more susceptible to pain from an old injury or to the development of new problems, such as early arthritis.
The Wear and Tear: Repetitive Stress and Degeneration
Many injuries, particularly those from repetitive motion injuries like those accounting for approximately 28% of all serious work-related injuries and illnesses in private industry, are not the result of a single traumatic event. Instead, they accrue over time due to constant, low-level stress. This repetitive micro-trauma can lead to tissue and joint degeneration, making them more prone to the persistent discomfort of an old injury.
The Brain's Blueprint: The Nervous System's Role in Chronic Pain
The brain plays a critical role in how we perceive and experience pain. It's not just a passive recipient of signals but an active interpreter. When pain returns, it often becomes chronic.
Pain's Memory: When the Nervous System Learns to Be Chronic
Through a process known as central sensitization, the nervous system can become hypersensitive, essentially learning to be in a state of chronic pain. This means that when pain returns, the pain signals can be amplified, and discomfort can persist even when the original tissue damage has healed. The brain remembers the pain, making it easier to trigger again.
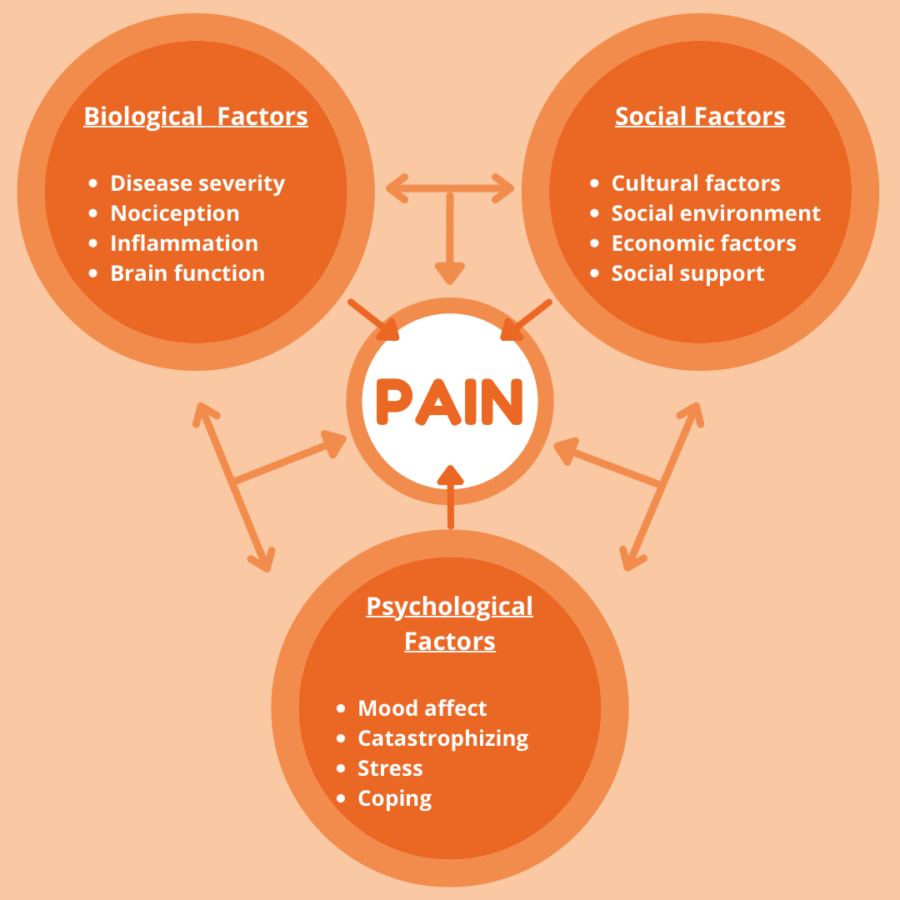
The Invisible Burden: Psychological Factors and Pain Perception
The mind-body connection is undeniable. Stress, anxiety, and depression can significantly amplify pain perception. Furthermore, the fear of re-injury can lead to avoidance behaviors, causing deconditioning and making individuals more vulnerable. It’s well documented that injured workers develop depression 45% more often than their uninjured coworkers, demonstrating the profound psychological impact on recovery.
External Influences: Lifestyle, Environment, and Daily Habits
Our daily lives and surroundings can contribute to or exacerbate persistent pain. If pain returns, it may be time to make some changes.
Daily Habits and Ergonomics: The Unseen Perpetuators
Prolonged sitting, poor posture at a desk, improper lifting techniques, or repetitive motions in daily tasks can all place ongoing stress on the body. These habits can aggravate an old injury or create new biomechanical issues that perpetuate discomfort.
Fueling or Hindering: Nutrition, Hydration, and Sleep
What we consume and how we rest directly impact our body's ability to heal and function. A diet high in inflammatory foods can worsen chronic inflammation, while dehydration can impair tissue health. Inadequate sleep deprives the body of crucial recovery time, hindering the repair processes essential for lasting healing and optimal performance.
Environmental Factors: The Weather's Whisper
For some, changes in weather, such as fluctuations in barometric pressure or humidity, can influence joint pain and muscle stiffness. While not a root cause, these external factors can sometimes trigger or amplify discomfort associated with an underlying, unaddressed injury.
Unmasking Your Own Hidden Causes: A Path to Self-Awareness
Understanding these hidden causes empowers you to become an active participant in your recovery when your pain returns.
Becoming Your Body's Detective: Self-Assessment Questions
Ask yourself: Does my pain worsen with specific movements or prolonged positions? Do I notice a "tightness" or restricted mobility beyond the initial injury site? Are my muscles consistently fatigued or sore in areas other than the original injury? Have I made significant changes to my lifestyle or work environment recently?
Recognizing the Red Flags: When to Listen to Your Body
Persistent discomfort that doesn't improve with basic rest, pain that radiates or changes character, recurring inflammation, or a noticeable loss of mobility or strength are all red flags indicating that deeper issues may be at play.
The Professional Perspective: Expert Guidance for Lasting Recovery
Addressing persistent pain requires a comprehensive approach that goes beyond simply managing symptoms.
Beyond Symptom Management: Comprehensive Diagnosis and Assessment
Effective recovery begins with identifying the specific hidden causes contributing to your discomfort. This often involves a thorough assessment by healthcare professionals.
A Toolbox of Solutions: Integrated Treatment Approaches
A multidisciplinary approach is often most effective. This can include:
Physical Therapy: Focusing on restoring mobility, strength, and proper movement patterns. Therapists can identify and address muscle imbalances, retrain faulty movement mechanics, address biomechanical issues, improve joint function, and help manage pain.
Chiropractic Care: Addressing structural and biomechanical issues, spinal alignment, and joint function, which can alleviate stress on injured areas and the nervous system.
Manual Therapy: Techniques to address scar tissue, adhesions, joint restrictions, muscle tension, and movement patterns.
Pain Management Specialists: For persistent nerve-related pain or chronic inflammation.
Lifestyle Coaching: Guidance on nutrition, sleep, and stress management.
Reclaiming Your Body: Strategies for Sustainable Healing
Lasting recovery is about rebuilding resilience and preventing future relapses.
Building Resilience: Strength, Mobility, and Stability
A robust recovery program focuses on regaining full strength and mobility in the injured area and surrounding muscles. Improving stability, particularly in the core and hips, is crucial for supporting the entire body and preventing compensatory strain.
Long-Term Wellness: Lifestyle Adjustments and Preventive Care
Integrating healthy habits into your daily life, such as proper ergonomics, regular exercise that includes a balance of strength and flexibility, mindful nutrition, and adequate sleep, is key to maintaining your recovery and preventing the return of pain.
The Power of Partnership: Working with Your Healthcare Team
True healing is a collaborative journey. By partnering with your healthcare providers and actively engaging in your recovery, you can unmask the hidden causes of your persistent pain and achieve sustainable, long-term relief, ultimately improving your overall quality of life and performance.
What to Takeaway
The frustration of an injury that won't stay gone is a signal that the body's healing story is more intricate than it first appears. While acute pain may subside, underlying issues such as problematic scar tissue, nerve sensitivity, chronic inflammation, biomechanical imbalances, and even psychological factors can keep the cycle of discomfort alive. Recognizing these hidden causes is the first step toward effective and lasting recovery. By shifting focus from mere symptom management to a comprehensive understanding of your body's unique biomechanics and nervous system responses, you can move beyond surface-level healing. Engaging with healthcare professionals, embracing integrated treatment approaches, and committing to sustainable lifestyle adjustments are crucial for rebuilding resilience. Ultimately, reclaiming your body and achieving proper recovery means becoming an active detective of your own health, understanding the whispers of discomfort, and working collaboratively to silence the echoes of old injuries for good.